What is febrile seizure?
Febrile seizures are seizures that occur between the ages of 6 and 60 mo (peak 12-18 mo) with a temperature of 38°C (100.4°F) or higher, that are not the result of CNS infection or any metabolic imbalance, and that occur in the absence of a history of prior afebrile seizures.
What are the types febrile seizure?
A simple febrile seizure is a primary generalized, usually tonic-clonic, attack associated with fever, lasting for a maximum of 15 min, and not recurrent within a 24-hr period.
A complex febrile seizure is more prolonged (>15 min), and/or is focal, and/or recurs within 24 hr. Febrile status epilepticus is a febrile seizure lasting longer than 30 min.
What is the effect of simple febrile seizure?
There are no long-term adverse effects of having one or more simple febrile seizures. Compared with age-matched controls, patients with febrile seizures do not have any increase in the incidence of abnormalities of behavior, scholastic performance, neurocognitive function, or attention.
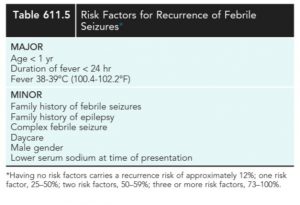
What is the chance of recurrence?
Children who develop later epilepsy, however, might experience such difficulties. Febrile seizures recur in approximately 30% of those experiencing a first episode, in 50% after two or more episodes, and in 50% of infants younger than 1 yr of age at febrile seizure onset
What are the risk factors for recurrence?
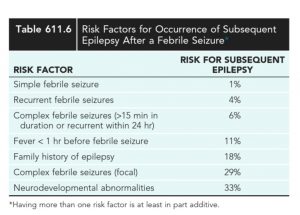
What is the risk of epilepsy?
What is the genetics of febrile seizure?
T he genetic contribution to the incidence of febrile seizures is manifested by a positive family history for febrile seizures in many patients. In some families, the disorder is inherited as an autosomal dominant trait, and multiple single genes that cause the disorder have been identified in such families.
. Genes associated with febrile seizures include SCN1A, SCN1B, SCN9A, and CPA6.
Which all epilepsies are preceeded by febrile seizure?
Almost any type of epilepsy can be preceded by febrile seizures. A few epilepsy syndromes typically start with febrile seizures; these are generalized epilepsy with febrile seizures plus (GEFS+), severe myoclonic epilepsy of infancy (SMEI or Dravet syndrome), and, in many patients, temporal lobe epilepsy secondary to mesial temporal sclerosis
Which all infections is associated with febrile seizure?
Febrile seizures often occur in the context of otitis media; roseola and
human herpesvirus (HHV) 6 infections; and infections with norovirus, enteroviruses, Shigella, or similar agents, making the evaluation more demanding. In patients with febrile status epilepticus, HHV-6B (more frequently) and HHV-7 infections account for 30% of the cases.
When should we do lumbar puncture?
Meningitis should be considered in the differential diagnosis, and lumbar puncture should be performed for all infants younger than 6 mo of age who present with fever and seizure, if the child is ill-appearing, or at any age if there are clinical signs or symptoms of concern.
A lumbar puncture is an option in a child 6-12 mo of age who is deficient in Haemophilus influenzae type b and Streptococcus pneumoniae immunizations or for whom the immunization status is unknown.
A lumbar puncture is an option in children who have been pretreated with antibiotics
What is the role.of EEG?
If the child is presenting with the first simple febrile seizure and is otherwise neurologically healthy, an EEG need not be performed as part of the evaluation.
An EEG would not predict the future recurrence of febrile seizures or epilepsy even if the result is abnormal. Spikes during drowsiness are often seen in children with febrile seizures, particularly those older than age 4 yr, and these do not predict later epilepsy.
EEGs performed within 2 wk of a febrile seizure often have nonspecific slowing, usually posteriorly. Thus, in many cases, if an EEG is indicated, it is delayed until or repeated after more than 2 wk have passed.
An EEG should, therefore, generally be restricted to special cases in which epilepsy is highly suspected
What is the role of neuroimaging?
Neuroimaging A CT or MRI is not recommended in evaluating the child after a first simple febrile seizure. The workup of children with complex febrile
seizures needs to be individualized. This can include an EEG and neuroimaging, particularly if the child is neurologically abnormal.
Approximately 10% of children with febrile status epilepticus are reported to have unilateral or, less frequently, bilateral swelling of their hippocampus acutely; subsequent long-term hippocampal atrophy is evident in about 71% of those who had the acute findings
. Whether these patients will ultimately develop temporal lobe epilepsy remains to be determined.
What is the treatment?
n general, antiepileptic therapy, continuous or intermittent, is not recommended for children with one or more simple febrile seizures.
Parents should be counseled about the relative risks of recurrence of febrile seizures and recurrence of epilepsy, educated on how to handle a seizure acutely, and given emotional support.
If the seizure lasts for longer than 5 min, acute treatment with lorazepam, midazolam, or diazepam .
Rectal diazepam is often prescribed to families to be used at home as a rescue medication if a febrile seizure lasts longer than 5 min ().
Alternatively, buccal or intranasal midazolam may be used. In cases of frequently recurring febrile seizures, intermittent oral clonazepam (0.01 mg/kg every 8-12 hr up to a maximum dose of 1.5 mg/day) or oral diazepam (0.33 mg/kg every 8 hr) can be given during febrile illnesses.
Such therapies help reduce, but do not eliminate, the risks of recurrence of febrile seizure




 Superintendent, ICH.
Superintendent, ICH.